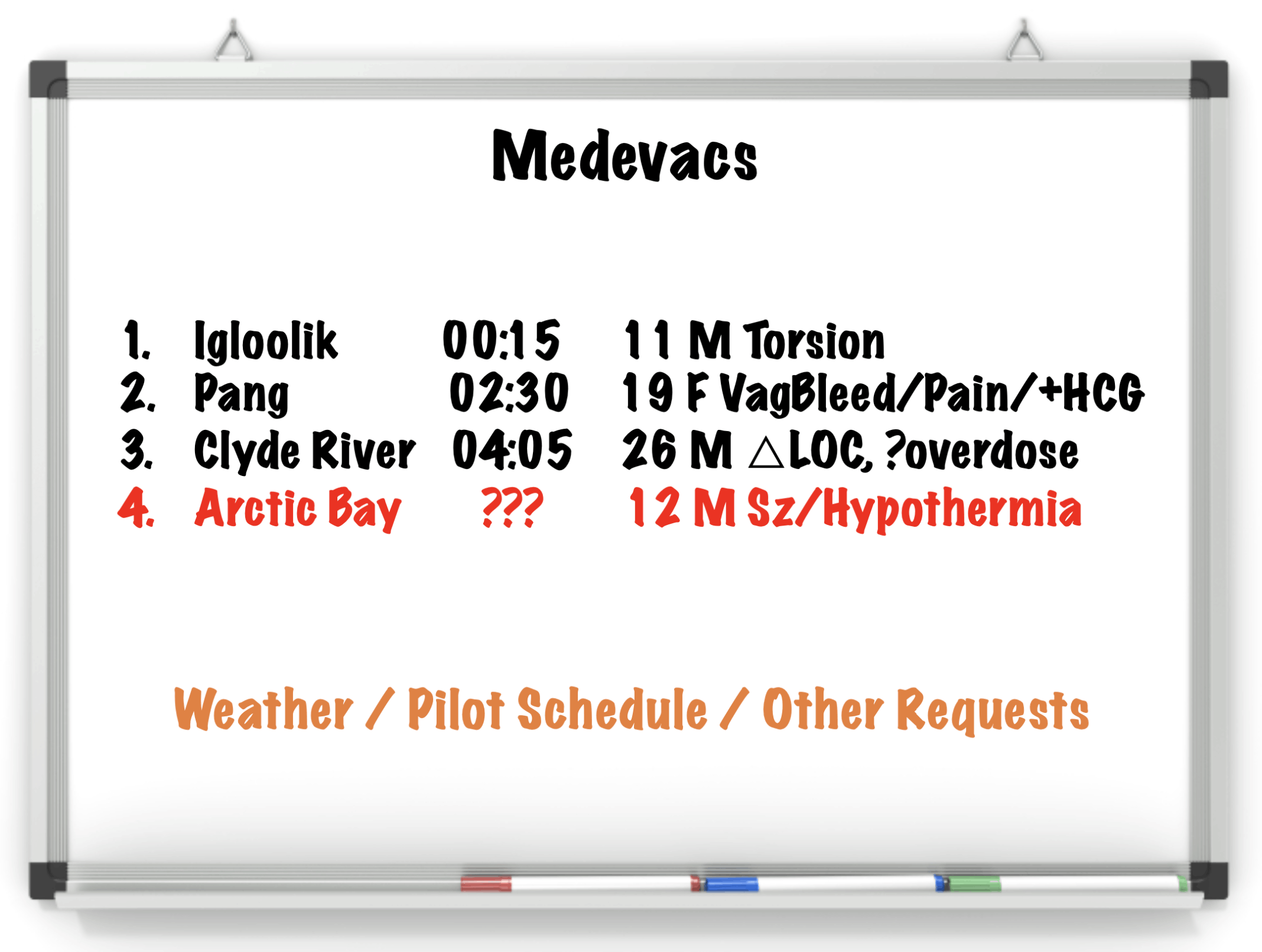
Case
EMS transport – no pre-alert came in ventilating patient
- Witness seizure approx. 1min
- Took photos of medications - - Ramipril, allopurinol, Jardiance, nifedipine
Call in additional support – General Practitioner Anesthesiologist (GPA), emerge RN and two LPNs and had to call in lab and x-ray
Defibrillator Pads place and IV's started
Airway - as per EMS - NPA difficulty bagging as patient has large neck with vomit everywhere with SPO2 in upper 80s
Breathing – looks deep and rapid (kussmauls) course and decreased to bases bilaterally
Circulation – hypertensive 195/110 p 130s warm extremities and afebrile
GCS 3 – pupils 2mm minimally reactive
BGL – unreadably high
No obvious injury
General seizure starts
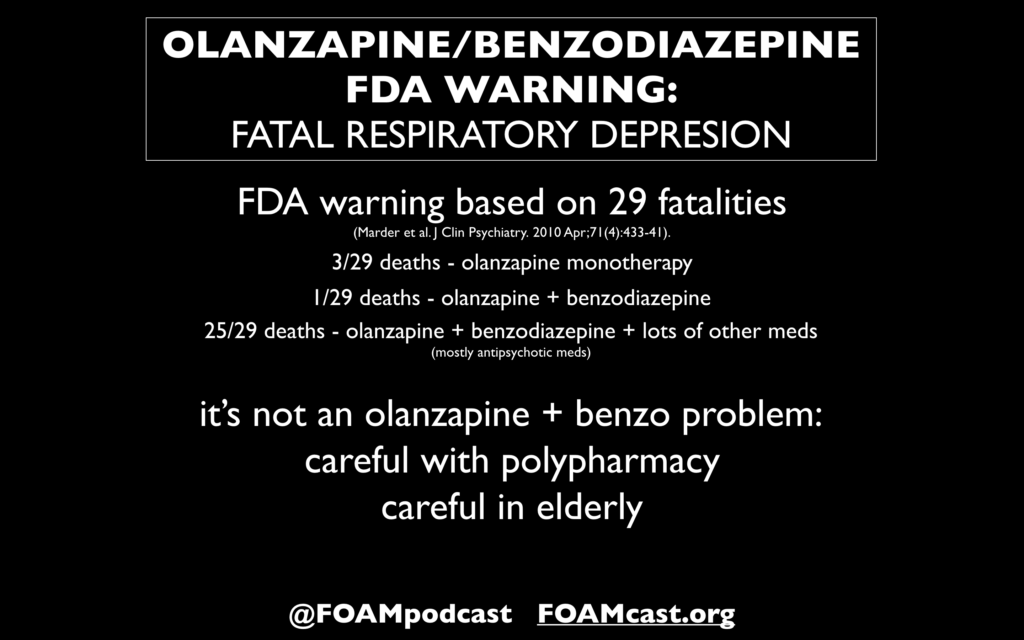
- Ativan 4mg IV followed by another 4mg dose given 4 min later
- Phenytoin 20mg/kg – seizure stop
Total seizure 5 min. Patient hypoxia – blue in color difficult to ventilate
LABS - VBG, glucose, electrolytes, osmolality, LFT, CBC, tox screen, CK, creatinine, and lactate
ECG – narrow sinus tach and QTC 570 no ST-elevation
3 total IVs placed
Family arrives but provides minimal information other than states patient doesn’t drink much alcohol
☙ Priority is to manage Airway
- Fluids
- Vasopressors – norepinephrine
- Equipment
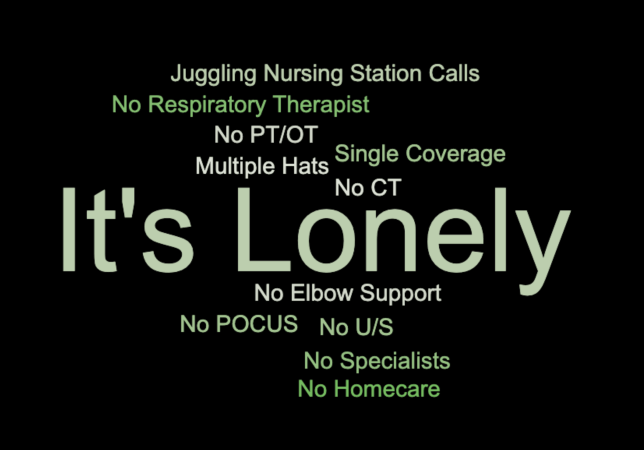
☙ Consider the challenge of staff and their scope of practice from RN to LPN and try not to overtask anyone
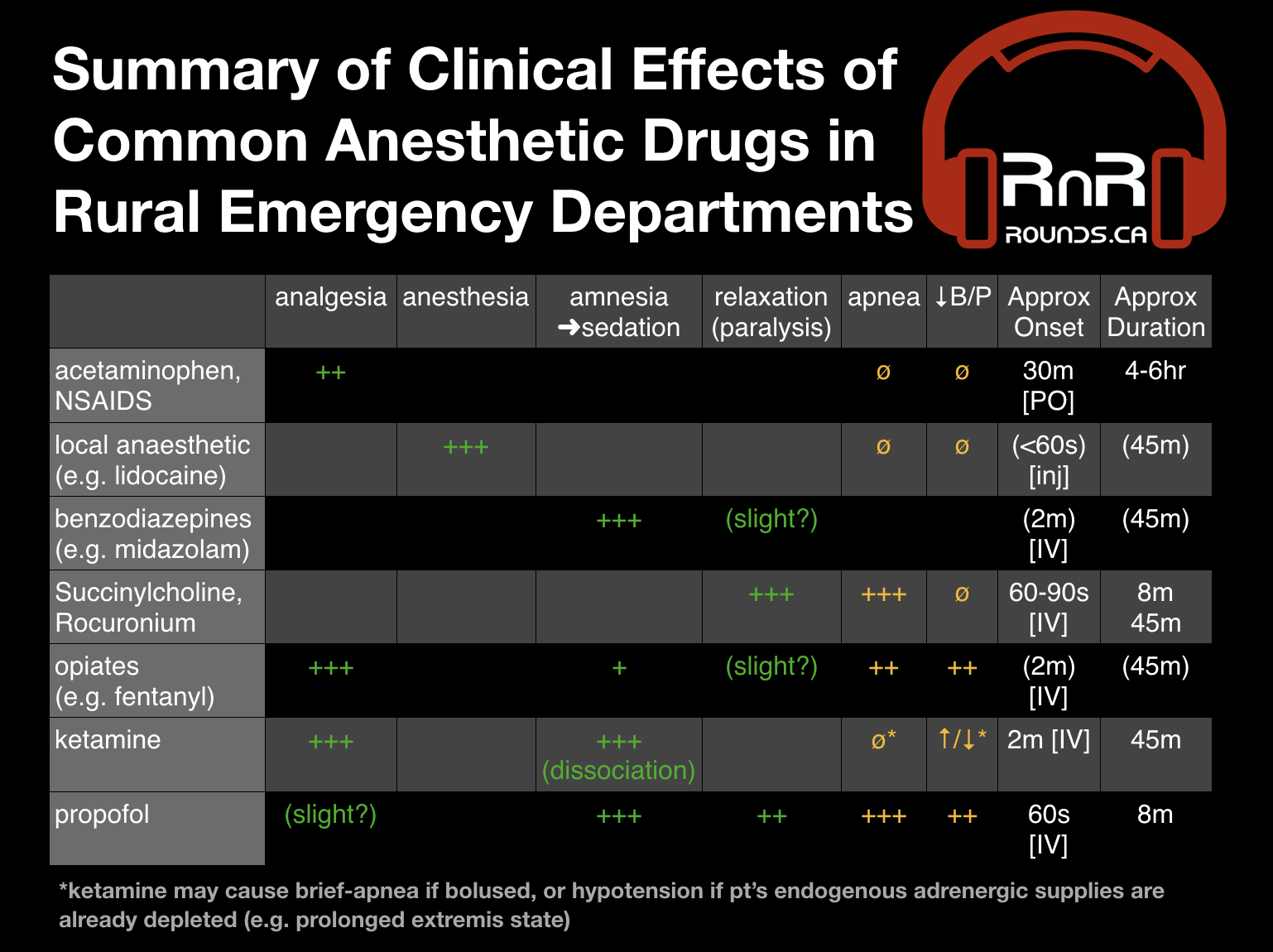
GPA – intubate – no paralytics or pre- procedural sedation
- Started propofol post intubation
Blood gas – pH6.8, bicarb 8, lactate >20 – No PaCO2 available
Consult with transport Doc – who is also helping with pt management
Vitals Pulse 130s, BP 130/80, post intubation SPO2 92% on ventilator PEEP at 5 with increased RESP rate to blow off acid.
Secondary survey – unremarkable except continue course bilateral breath sounds.
BP decreases 80/50s
- Pressure bag of normal saline
- Pressors - norepi - 0.1mg/kg/h
Setting up ART line and central line being set up
More labs
WBC – 20
Hemoglobin – normal
Na – 133
K – 3.9
Anion 39
Creatinine 159
Glucose 51
Lactate 25
LFT normal
Serum osmolality – 365 (results received next day)
Chest x-ray - no consolidation
Start DKA protocol – most centres have printed form.
- Monitor potassium and supplement
- Monitor fluid resuscitation
- Insulin infusion - 0.1Unit/kg/h
- Monitor electrolytes and anion gap regularly.
- Cover infection – Piperacillin/Tazobactam
- Consider treating alcohol poisoning – Fomepizole
Limited number of people to admin med and IV routes. Need to prioritize order.
Another Seizure
- 4mg IV Ativan
- Keppra Loading dose drawn up
Repeat Blood gas – pH 7.17, bicarb 13, and lactate 15. BGL still unreadably high
ART and central line in
Vitals stable. Improvement with metabolic acidosis.
Transport considerations
- Two provinces on the call
- No air helicopter
- No flights
- Only ground transport
- Decision was to send ground ambulance with GPA to meet with specialized team.
Repeat Blood gas – pH 7.22, Bicarb – 17, Lactate – 10
Chest x-ray – confirm central line, Foley catheter, Check all IVs to ensure patency.
5 days in ICU. 8 days in medical ward
LP, EEG, CT Head – normal. Thing seizures were from severe DKA. Did end up with aspiration pneumonia.
Treated for Type 2 diabetes – A1c - 16. Was previously being treated months prior but stopped because he didn’t want to take meds anymore.
Resources
- EM cases podcast and summaries used to help with resuscitation
- Resuscitation crisis manual
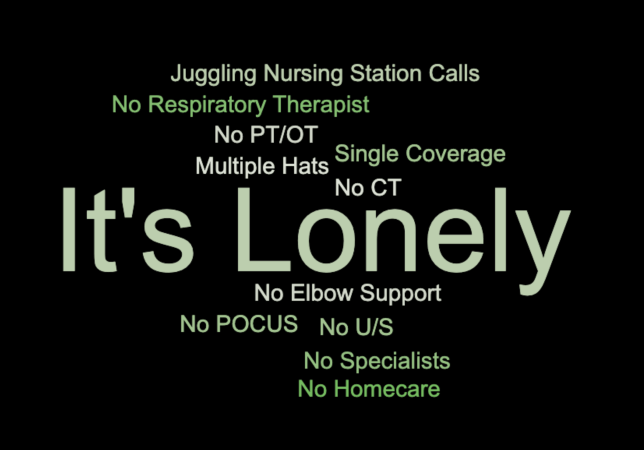
Reflection/challenges
- Nursing allocation of task
o Close loop communication
o Don’t overwhelm with multiple orders at a time
- Prioritizing tasks
o Limited people and interventions
o Would have wanted more fluid resuscitation, got sidetracked with seizures/other medical problems.
- Communicating between team and specialist on phone
o Multiple people on call
o Spotty services
- Multitasking
o No time or space to reflect on what is happening
- Deciding when and how to transport the pt
o Hard without air support