
Volume 03:
Episodes 051 - 075

Episodes 051 - 075
Published 14 November 2023
https://podcasters.spotify.com/pod/show/jonathan-wallace-md/episodes/075-Tox-1-Fever--Rigidity-e2bplp8

Case 2
36-week G2P1 followed by obstetrics due to placenta previa.
Came in with bright red painless bleeding initially hemodynamically stable. Site capable of obstetric support.
BP mid-90s HR 120s – concerned with significant blood loss - ATLS - Class 3 shock 30-40% circulating blood loss – unsure if validated for pregnant women – considered for this case to estimate blood loss.
Pressure infused first unit of O-neg blood, 1g TXA given - second unit infused on route with EMS - receiving hospital 25min away
If longer transport and site has surgical capabilities, consider surgical intervention before transport.
Perimortem c-section – last ditched effort.
Get consult with expert ASAP to have them on hand to work through case.
*Speed is of the essence in cases of bleeding. TXA 1g IV over 10min loading dose. Consider a second dose as per local protocol if the patient is going to stay for longer. Consider what options for blood products are in your area*

Published 13 October 2023



Published 12 Aug 2023



Published 2 Apr 2023
https://spotifyanchor-web.app.link/e/LBnaKiorCyb

Published: 1 Apr 2023
https://podcasters.spotify.com/pod/show/jonathan-wallace-md/episodes/Pediatric-Potpourri-finger-nail--nasal-FB--H-A-T---intranasal-sedation-e20bevj
Avulsed Fingernail
4yo female finger slammed in door. Nail pulled distally out from nail bed from proximal nail fold. Nail intact but shifted.
Consult with plastic surgeon – don’t need to do anything. Conservative measures due to nail matrix likely to be intact. Keep wound clean and dry, wash with soap and water, wrap with cling gauze.
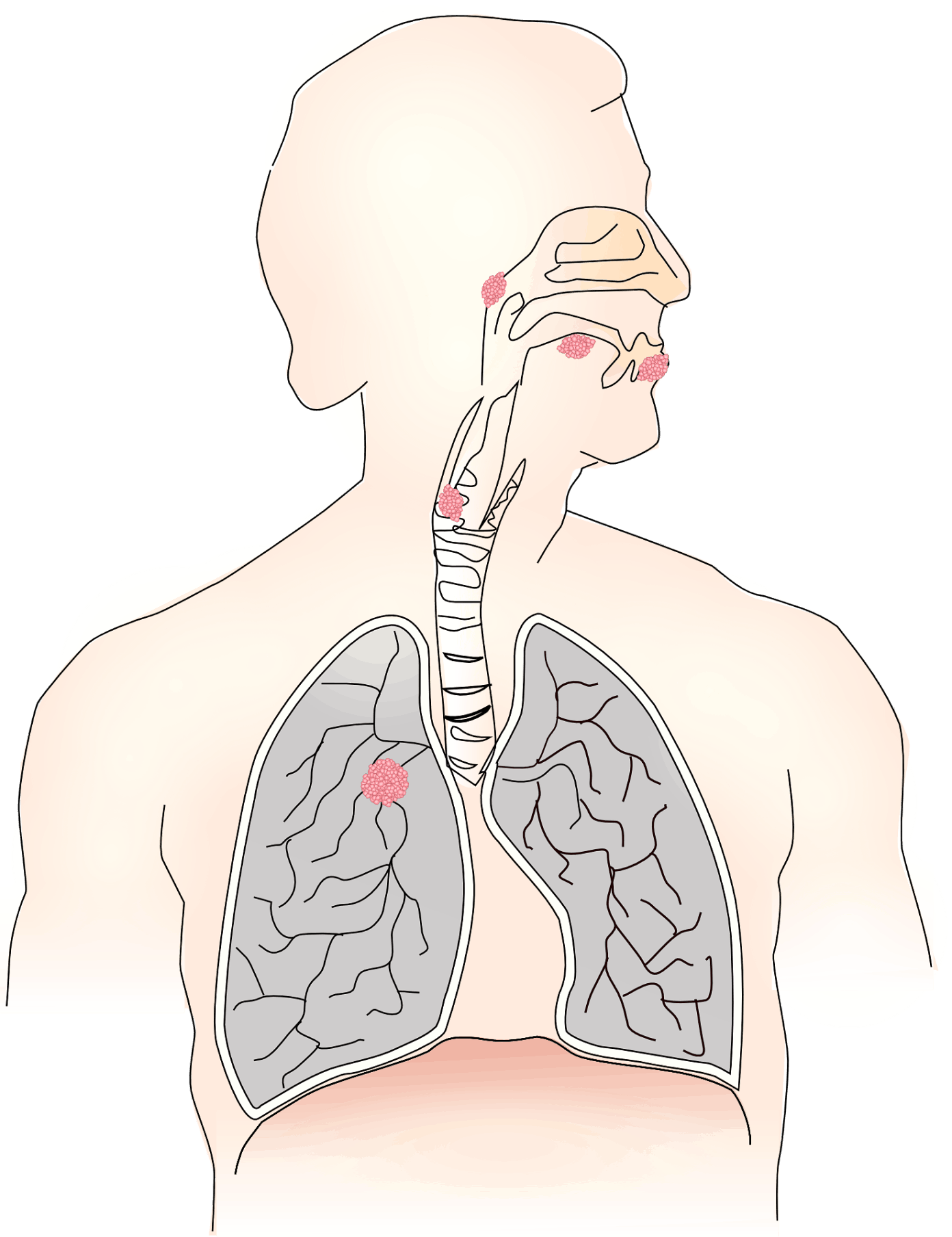
Nasal Foreign body
2 ½ year old with Styrofoam up nose.
Typical treatment is for parent to do mouth to mouth while obstructing unaffected nare. Causes startle response and glottis to close allowing for pressure to build up behind foreign body to pop it out – very effective.
Parents attempted mouth to mouth with no effect, tried to hook it and did not help.
Consult ENT – recommended leaving foreign body in for a week and allow for mucous to coat foreign body (cautioned it would start to smell) to allow for it to be removed without worrying it would break apart.
Head Laceration
PECARN - MD Calc website tells risk – if imaging, monitoring, or nothing.
Leave print out with parents on how to manage head injuries.
HAT - Hair Apposition Technique – use hair to close wound and apply skin glue
https://www.youtube.com/watch?v=Aj9chhWJfPo&ab_channel=BrianLin
Pediatric sedation – Intranasal ketamine and some screen time
The younger the patient the higher the amount of anesthetic
3-9mg/kg – the more upset they are the higher the starting dose

Published 5 Mar 2023
https://anchor.fm/jonathan-wallace-md/episodes/Drowning-w-Dr-Nour-Khatib-e1vqh6k


Published 3 Feb 2023
https://spotifyanchor-web.app.link/e/ke8Ss7FK7wb
https://www.ncbi.nlm.nih.gov/books/NBK544284/
https://www.youtube.com/watch?v=XXp0EtKtlF8&ab_channel=EM%3ARAPProductions
https://www.youtube.com/watch?v=H2Sj1v_yDVU&ab_channel=Traumavideo

Published 24 Jan 2023
https://spotifyanchor-web.app.link/e/QCgt5xCK7wb

Published 9 Jan 2023
https://spotifyanchor-web.app.link/e/LE9xnAEK7wb
Published: 9 Dec 2022
https://spotifyanchor-web.app.link/e/HPeDxZvEHvb
Contents & Timing
00:20 Learning Objectives
01:00 Disclosures + Course / Fellowship List
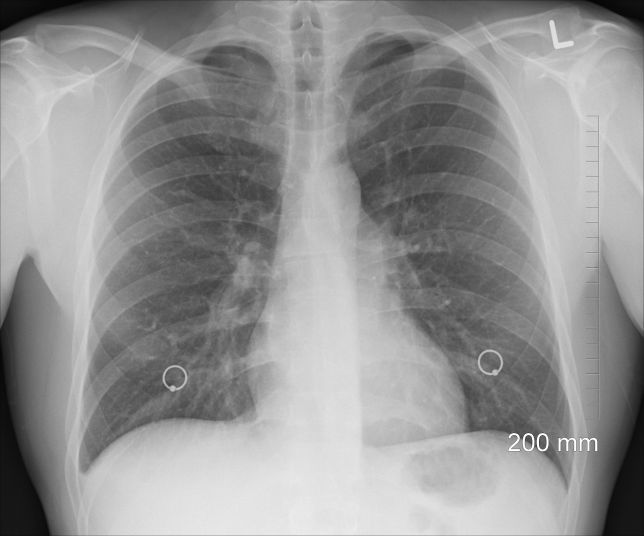
02:10 Overview of Rural PoCUS Education Opportunities in Canada (as of Dec 2022)
06:15 "Case Rounds" (10 actual Rural Cases & how comprehensive PoCUS played a role)
55:35 HIGHEST VALUE: Take Home Points
56:45 Advice for how YOU might best proceed with future PoCUS education
